LearningWho's Responsible?
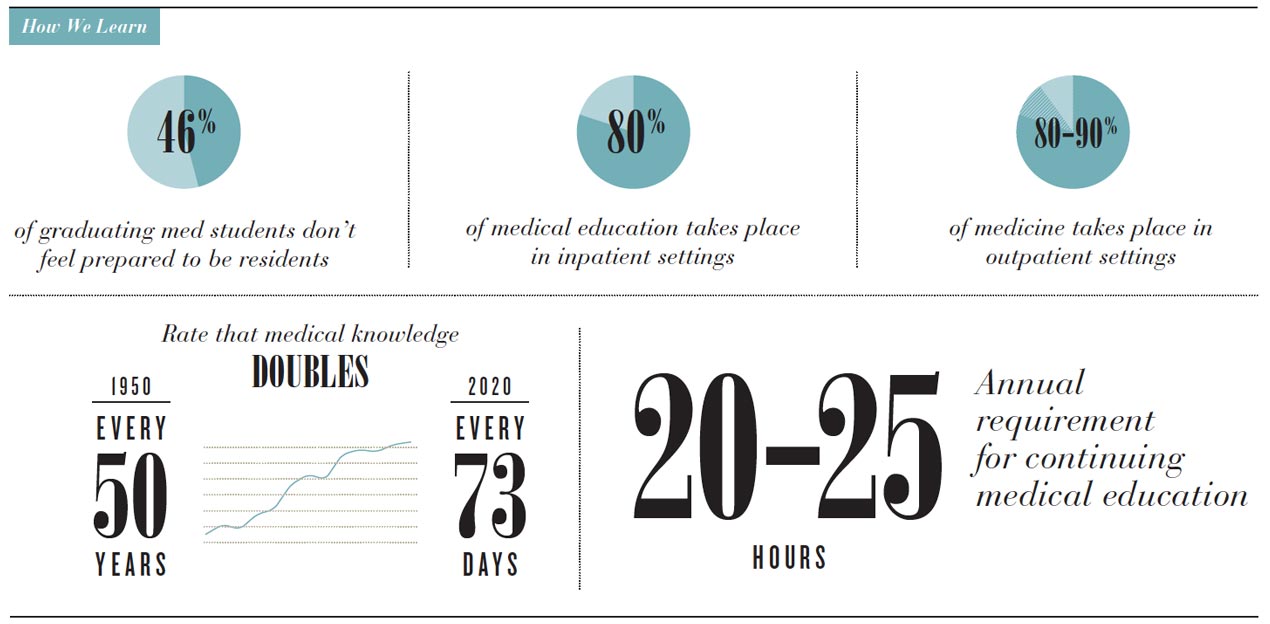
With biomedical knowledge compounding every minute, there’s no way for our human brains to sort through it all. New tools, innovative curriculums and even robots will only get us so far. We’ll need a culture of continual learning and people to model how to embrace a brave new future.
There. He’d said it. He hadn’t opened up his textbooks since the second week of medical school. It was June and quick math proved that they had stayed shut virtually the entire year. In his excitement, the new medical school graduate seemed as if he’d momentarily forgotten that every dean and chair of the School of Medicine were sitting around the tables of the first-ever educational retreat.
After the student finished his passionate educational testimonial, there were a couple audible sighs, one “what-a-shame” comment, and several “good-on-you” cheers for his courage and honesty.
But no one in the room could deny the truth: The model we’ve used for training medical students for the past 100 years is out of sync, not only with how this generation learns, but also how they will practice medicine. “Even as I’m learning some things, like how to do a physical exam, I think to myself, ‘I know this isn’t how we’re going to do it after I graduate,’” says Matthew Petersen, a third-year medical student at the University of Utah School of Medicine. “Medical knowledge should come with a ‘best if used by’ warning label,” says Sara Lamb, M.D., associate dean for curriculum. She’s only half-joking. It’s estimated there are 1 million articles published in PubMed annually. “The lecture we give today will likely need to be updated the next semester.”
It’s not only what they learn, but also how they learn. “The days of Power-Point slides and big lectures are over,” says Senior Vice President for Health Sciences Vivian S. Lee, M.D., Ph.D., M.B.A. “This is the Khan Academy generation of students.” Today’s future doctors are more likely to skip class and find an online video, interactive memory puzzle or question bank to prepare for the test. Schools are trying to figure out how to flip the classroom, embrace simulation, train in teams and foster lifelong learning. The Cleveland Clinic is partnering with Microsoft to teach anatomy through holographic virtual reality. Watson, IBM’s cognitive supercomputer, is in his third year of medical school, with the homework assignment of figuring out how to train doctors better. But even the fanciest new learning platforms and the most aggressive curriculum reform still will not prepare students for the onslaught of information or the team-based, precision- medicine-focused, value-driven world they’ll soon be entering.
“We need to ask ourselves, given the current health care landscape, are we being accountable?” says Tony Tsai, M.B.A., School of Medicine education strategy director. Are the graduates we’re producing prepared to have an optimal effect on health?
Faculty across disciplines complain that students only care about learning the material they will be tested on. They regret they don’t ask questions, lack curiosity, aren’t deep thinkers or high-level problem solvers. Stressedout students respond there’s no time for that. “We are so overwhelmed with mastering the basics, that going deeper into content is a luxury we can’t afford,” says third-year medical student Curtis Sudbury.
No doubt, students will need to take more personal responsibility for their learning. But in the real world of patient care, there will be no one to blame for not telling them what they needed to know. So what’s the role we play in creating a safe environment for inquiry? Are we measuring their success in a way that shows we value curiosity and mastery over knowing and competency? Or have we designed a system that has them stuck in survival mode.
Focusing on Culture
For Tsai, fixing education is really about culture change. “There’s a lot of churning of curriculums without a lot of transformation,” he says. Tackling the informal and hidden curriculums—the social structure and unspoken rules that guide how providers work with each other—may be the more urgent challenge.
“As a medical student, what we think is important is whatever our attendings tell us is important,” says Petersen. If no one’s talking about bundled payments, disparities and population health, or the importance of having difficult conversations about palliative care, Petersen says, there’s no reason to think we should care.
We need role models who have already embraced the future, dedicated themselves to continual learning and taken responsibility for preparing those who will follow. “If we choose to work in an academic setting, then everything we do should be about teaching and modeling, not just for the small group of students rotating through, but for every student, resident or trainee at the institution,” says Lee. That kind of environment doesn’t just happen organically. It requires a culture that doesn’t relegate learning to students and classrooms but provides trainees, faculty and staff the opportunity and resources to learn new skills. Just as we strive to personalize care for patients, we need to personalize education—and tap into passion and curiosity.
“I’ve never met a provider who doesn’t care about patients or want to improve the way we deliver care,” says Chrissy Daniels, M.S., director of strategic initiatives. We just need to tap into that core intrinsic motivation and provide the resources and support they need to do it. “Taking on improving a huge system can feel like summiting Everest. And no one can summit Everest alone,” says Daniels. We need to supply engaged staff with Sherpas. At University of Utah Health, those resources range from an hour-long online course in Lean training to a semester-long leadership development project. More than 1,000 staff and faculty have logged on or signed up for face-to-face training seminars. And they keep coming back. Collectively, they’ve developed more than 750 value projects, 180 measures of quality, more than 100 tests of service and 109 cost benchmarks.
Modeling For Millennials
“When I ask students, ‘How many of you came into health care thinking that you were going to be part of significant change?’ they all raise their hands,” says Lee. “They want this transformation, even crave it. So now it’s our responsibility to figure out how to tap into the true strengths of this generation.” Tsai agrees. Unlike past generations, who were willing to put in the time, millennials are ready to get going. But they need a cause. They want to go toward meaning, he says. And they need their role models to reassure them, to show them it’s important, to give them permission.
“The number one thing is for learning to be inspiring—for students and faculty alike,” says Lamb. And there’s nothing more inspiring than having mentors who are passionate. So instead of focusing on curriculum design, we’re celebrating people who are already there. They’ve taken on the responsibility to learn new skills and are helping create a system that supports that kind of learning for others. They’re changing the culture.