CATALYSTS FOR CHANGE

Faster, cheaper DNA sequencing is sparking optimism that cures are just around the corner. But to turn genetic data into knowledge that’s meaningful for patients, we need experts with wildly different skill sets to connect with one another. Academic medical centers are singularly poised to help foster those collaborations, and at the University of Utah, that’s what we do best. Here we highlight just some of the brilliant minds who are forging new paths to discovery.
THE PHYSICIAN-SCIENTIST
aJoshua D. Schiffman, M.D., Associate Professor, Pediatrics; Adjunct Associate Professor, Oncological Sciences
“When we have a child in front of us who is sick and dying, we intuitively focus on treatment – not genetic risk,” says pediatric oncologist Joshua Schiffman, M.D. He believes that eradicating cancer – his ambitious goal – will require us to expand that clinical focus to include a hereditary mindset. “Heart disease, diabetes, even gout – we’re learning now that almost every disease has some sort of genetic basis.” At Schiffman’s urging, a family history is now taken on every child with cancer in Utah. Families with enhanced risk are referred for preventive screening or enrolled in research, yielding new discoveries that may point the way to targeted treatments and cures. “I was trained first as a general pediatrician, and as a pediatrician we try to prevent disease,” he says. “I wake up every morning thinking about how I can bring together people, resources and expertise to do that.”
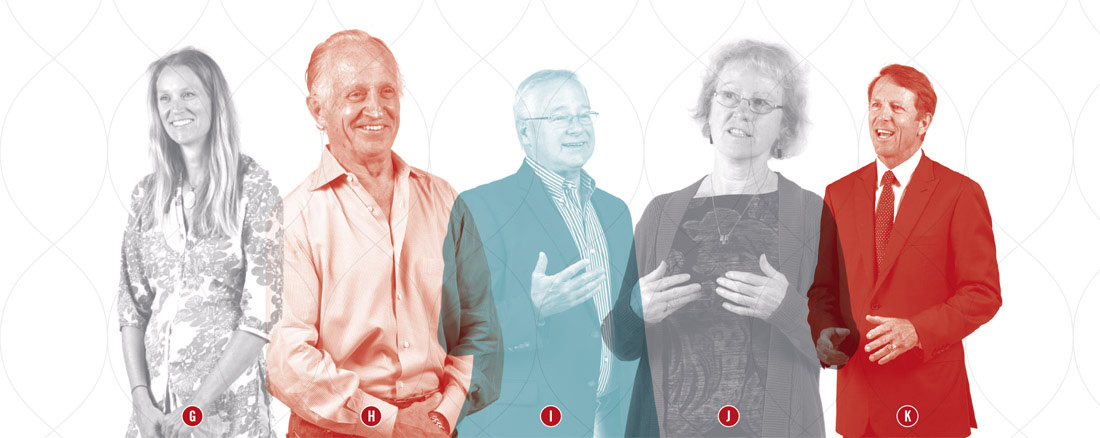
THE CONNECTORS
bDeborah Neklason, Ph.D., Research Associate Professor, Internal Medicine
cLynn Jorde, Ph.D., Chair, Department of Human Genetics
Astute specialists often make clinical observations that hint at genetic causes but lack the training or resources to act. “They need to be in an environment that encourages a research perspective,” says Deborah Neklason, Ph.D., program director for the Utah Genome Project (UGP). Neklason and Executive Director Lynn Jorde, Ph.D., spearhead efforts that link physicians and scientists with informaticists, epidemiologists and geneticists, and assist them in using a powerful resource – the Utah Population Database – to find what they’re looking for. In two years, UGP research has, so far, identified new risk factors for preterm birth, heart arrhythmia, immunodeficiencies, breast cancer and the causes of three rare diseases, and developed new disease gene identification tools. Each success helps build a pipeline from DNA to diagnosis. “It’s a great leap forward for science, for genetics, for medicine and for the quality of life for families,” says Jorde.
THE METHODOLOGIST
dLisa A. Cannon-Albright, Ph.D., Chief, Division of Genetic Epidemiology; Professor, Internal Medicine
Utah’s genealogical riches have yielded discovery of dozens of disease-causing genes, including the breast cancer genes BRCA1 and BRCA2. “Those genes don’t explain all hereditary breast cancer,” says one of the geneticists credited for their discovery, Lisa Cannon-Albright, Ph.D. “What about all the other people who are at risk for breast cancer or other diseases, but we haven’t found the gene that explains their family’s risk?” While looking for new genetic signatures of disease, Albright develops algorithms, or recipes for calculating risk, based on family histories. She’s also working on a prototype of a national database for consumers to build their own health pedigrees matched to their medical records. “People say someday you’ll go the mall and give them a drop of blood and get your genomic profile. But for now the best indicator of risk for common disorders is a family history. We can do it today and it doesn’t cost you anything.”
THE ANALYSTS
eGabor Marth, D.Sc., Professor, Human Genetics
fMark Yandell, Ph.D., Professor, Human Genetics
If predictions hold, and the number of new genomes sequenced grows 20-fold in the next three years, we’ll have a big problem on our hands – the capacity to analyze them. That’s the impossible problem that Gabor Marth, D.Sc., and Mark Yandell, Ph.D., co-directors of the USTAR Center for Genetic Discovery, are trying to solve. “We are building an information highway that will be able to transport huge amounts of genetic DNA information from the sequencing machine to the clinic,” says Marth, who earned his chops on the 1,000 Genomes and other heavyweight projects. The duo develops genomic analysis software tools such as VAAST, which is used by more than 250 institutions worldwide. They’re collaborating with industry to build a user-friendly, web-accessible platform to distill genomic data into clinically relevant findings. “Our goal is to be able to go from DNA to diagnosis within minutes,” says Yandell.
THE TRANSLATOR
gKaren Eilbeck, Ph.D., M.Sc., Associate Professor, Biomedical Informatics
For all of their bright spots, computers are terrible at some things. Inference is one of them. If one scientist describes the location of a DNA variant as “chromosome 1” and another as, “chr 1,” computers won’t connect the dots. Multiply those kind of notation ambiguities by 3.5 million – the average number of variants in a person’s genome – feed them into software, and the result is a total genetic mishmash. “We can’t communicate if we’re not using the same language,” says informaticist Karen Eilbeck, Ph.D., M.Sc. To rein in the free-for-all, Eilbeck is working with people from the CDC, clinical laboratories, software development, accrediting agencies and research communities to create a worldwide standard. “Misinterpretation poisons the data. We can’t afford to let that happen.”
THE SCIENTIST
hMario Capecchi, Ph.D., Nobel Laureate; Distinguished Professor, Human Genetics
Finding a genetic mutation is just the beginning of the scientific story. One of the longest chapters to come is figuring out how changes in DNA spell trouble within the body. “If you formulate the questions appropriately, the answers will come,” says Mario Capecchi, Ph.D., distinguished professor of human genetics. He received the 2007 Nobel Prize for inventing gene targeting in mice, a revolutionary technique used by researchers around the globe to test how mutations morph into disease – the first step in uncovering novel treatments. “No story is one gene. It’s always the interaction of many genes together. It has a beginning, a middle and an end,” Capecchi says. “My end is always understanding.” Push understanding – push basic research – and translation, he says, will follow.
THE ETHICIST
iJeffrey R. Botkin, M.D., M.P.H., Professor, Pediatrics; Adjunct Professor, Human Genetics; Adjunct Professor, Internal Medicine
Should every newborn have his or her genome sequenced at birth and are we, as a society, prepared for what we might find? Genetics lets us visualize our bodies on the molecular level, revealing weaknesses that confer risk for various diseases. “But we don’t yet have the ability to intervene on many genetic conditions. So we have a gap between the ability to analyze this information and do something constructive about it,” says ethicist and pediatrician Jeffrey Botkin, M.D., M.P.H. Springing from this scientific challenge are ethical quandaries that Botkin – as a leading member of government advisory panels and director of the Utah Center for Excellence in the Ethical, Social and Legal implications of Genetics – is helping to anticipate. Botkin and his team craft tools for education and informed consent to guide families in choosing the right path. “This is a domain where there aren’t right or wrong answers.”
THE COUNSELOR
jBonnie Jeanne Baty, M.S., C.G.C., Professor, Pediatrics; Adjunct Professor, Nursing
Health providers are obligated to put the interests of the patient first, but genetic counselors treat the whole family, says Bonnie Baty, M.S., C.G.C., director of the graduate program in genetic counseling. They support patients along the emotional journey of comprehending not just their test results, but also how those results apply to loved ones. “We worry about the right to know, just as much as the right to not know.” The much-hyped promise of personalized medicine is driving up demand for genetic testing, and there’s a concern that we may have a national shortage of counselors to help interpret the results. Utah is insulated from the shortage due, in large part, to the pioneering work of Baty, the first genetic counselor in Utah, the first state to license counselors.
THE ADVOCATE
kMark Miller, CEO, Mark Miller Auto Group; Chair, University of Utah Hospitals and Clinics Board of Trustees; Chair, Utah Genome Project
With all the suffering in the world, why invest in genomics, a budding science with uncertain payoff? Why not spend your money on medical advances that are saving lives now – a new surgical technique or drug trial? Because sometimes you have to play the long game, says auto dealer and philanthropist Mark Miller of his decision to give a $250,000 seed grant to start the Utah Genome Project. The gift has sparked millions more in donations at a time when federal research funding wears thin, including $12 million from the California surgeon and entrepreneur Patrick Soon-Shiong, M.D., and his foundation. “If you pay attention to what’s going on in medicine, it’s clear genetics plays an important role,” Miller says. “We have such a huge opportunity to have a global impact on how we treat not just horrible diseases like cancer, but also common maladies, such as high cholesterol.”


