HOW CAN WE FIND RELEVANCE IN A LANDSCAPE THAT WON’T STOP SHIFTING?
Science is the pursuit of truth. What could be more clear-cut than that? Yet for today’s scientists, that search can be a winding, unsettling path through a constantly evolving landscape. Funding constraints, new trends and a growing emphasis on translation has investigators worrying there may be no place for them when the ground stops shaking. With their livelihoods hanging in the balance, they’re figuring out how to be adaptable and competitive, how to be open to eclectic partners and funding streams, and how to look at threats as opportunities to take science further than they imagined.
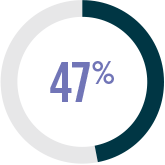
Funding for science has always been a moving target. Thirty years ago, we launched an all-out war on cancer, 15 years ago we were racing to sequence the first human genome, and now the nation’s capital is abuzz with the promise of precision medicine. Public health issues, the whims of politicians, the media, public perception and hard economic facts all mix together to shift priorities. Sprinkled into today’s recipe is the growing influence of patients, viral crowdfunding—think ALS Ice Bucket Challenge—and multimillion dollar, pink-ribbon campaigns.
“We are asking scientists to figure out new ways to work and align with the goals of the clinical system; now it’s our responsibility to create a system that supports and rewards that kind of work.”
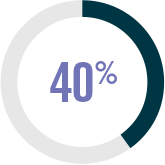
Carrie Byington, M.D., Associate Vice President for Faculty and Academic AffairsWhat captures the imagination of the public—or the NIH—doesn’t always match up with the most promising science or the impact of disease. In fact, when researchers analyzed NIH funding for 29 common conditions against the World Health Organization’s Global Burden of Disease data, they found there was only a moderate correlation. Conditions such as AIDS and diabetes came out funding winners while depression and chronic obstructive pulmonary disease came out on the losing side. Why? Good question. “Often, there’s no scientific rationale for funding or leaving certain areas,” admits Carl Thummel, Ph.D., professor of human genetics. He speaks from experience. NIH funding for his area of research—using the fruit fly to solve basic biological conundrums—has plummeted 30 percent in five years.
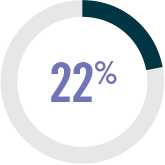
Unfortunately, there’s no discovery crystal ball to peer into, and when dollars are tight, as they are today, those fickle trends can make or break careers. With the NIH having lost about 22 percent of its purchasing power since 2003, many scientists consider it an all-out crisis, says Wesley Sundquist, Ph.D., co-chair of biochemistry. “Now when I go to conferences, people spend half of their time talking about how to get funding for their labs instead of their best scientific ideas.”
Whether or not we agree with the current funding trends, the simple fact is that we can’t afford to ignore them. And at the top of today’s priority list—for the NIH, venture capitalists, philanthropists and crowdfunders alike—is the potential to translate discovery into clinical applications. Translation gets a bad rap among some basic scientists, but is it really such a dirty word? “Improving human health through science is the mission of an academic medical center. That was the whole reason we decided to put hospitals and medical centers next to research-intensive enterprises,” says Dean Li, M.D., Ph.D., associate vice president for research.
A focus on translation doesn’t mean we shove basic science aside. It’s basic scientists who have the ability to affect more diseases than anyone else, says Li. “If we had said that every discovery had to be translated and every investigator had to translate, then we would have made a mistake based on the history of science.” How to recognize the drive for translational science while creating a fertile environment to make those fundamental discoveries, is today’s billion-dollar question.
Aligning the system
If we think about the translational mandate as less about the final product and more about creating the environment required to support translation, then the focus isn’t on directing science but on bridging institutional gaps. “We are asking scientists to figure out new ways to work and align with the goals of the clinical system; now it’s our responsibility to create a system that supports and rewards that kind of work,” says Carrie Byington, M.D., associate vice president for faculty and academic affairs. That means finding ways to lower the energy barrier to do translational work so that we protect researchers’ most valuable resource—time. Byington has been building a smorgasbord of resources to do just that through the Utah Center for Clinical and Translational Science, which she co-leads.
Because translational science moves across boundaries, it’s also made teamwork the new imperative. “No one individual holds all of the knowledge and expertise to tackle complex diseases,” says Mary Beckerle, Ph.D., CEO and director of Huntsman Cancer Institute. The power will come from disease-focused teams, something the cancer field has known for a decade. That brings with it another set of challenges for researchers whose success has been based around individual excellence, not on the ability to negotiate expectations, manage conflict and share both power and glory. “People are messy,” admits Beckerle. “And more people are messier.”
And who gets the credit for a groundbreaking discovery that involves a team of five or 30 or more? Genetic epidemiologist Hilary Coon, Ph.D., is one of hundreds of scientists in the Autism Sequencing Consortium that published a seminal Nature paper on the genetics of the disorder. “Bringing together an enormous quantity of data is making it possible to unravel new patterns that we couldn’t see otherwise,” she says. “Everybody in this consortium is more concerned with scientific progress than in making their name in the world.” While Coon’s altruistic attitude is admirable, the academic paradigm needs to catch up and reward contributions to a consortium, being a middle author and generously sharing data and samples. The University’s medical school recently revised its faculty appointment, retention and advancement guidelines to redefine excellence and reward team contributions, but Byington admits there’s a long way to go—institutionally and globally.
A New Kind of PI
A new breed of scientist has emerged to help guide colleagues through this changing world. Part institutional PI, part coach, part matchmaker, they’re forgoing the traditional lab route to become research administrators who can draw upon their scientific expertise to connect the right people, resources and knowledge. “I think this is one of the most promising pipelines for scientists and one of the most valuable resources for the institution,” says Senior Vice President Vivian Lee, M.D., Ph.D., M.B.A. “These are very smart, well-trained scientists who are thinking strategically and operationally about research.”
These research ambassadors are also tapping into philanthropic funding avenues and forging bold, new partnerships with the pharmaceutical and biotechnology industries. In two years, Amy Davis, Ph.D., director of research program development, has helped bring $20 million to a precision medicine initiative, the Utah Genome Project (UGP), and establish a partnership between UGP and the Regeneron Genetics Center (RGC). The collaboration is connecting five investigators who research autoimmune disorders to new resources and creating a pipeline to translate basic science discoveries into potential therapeutics. “We’ve put in years of work carefully characterizing symptoms and gathering patient samples,” says pulmonologist Mary Beth Scholand, M.D. “This partnership will help us get the answers that we—and our patients—are looking for, so we can act on them much more quickly.”
The Only Constant
Here’s what we can count on: Just when we figure out these funding trends, they will change again. Already there are signs that the pendulum is swinging back to basic science. Concerned by the decline in basic research, the NIH’s National Institute of Neurological Disorders and Stroke announced new funding for projects that aren’t explicitly disease-related. Politicians are changing too. For the first time in a decade representatives—from both sides of the aisle in the House and Senate—are calling for an NIH funding increase. And the field itself continues to evolve sparking funding announcements for new areas of research in cancer genomics, big data science and the use of mobile and personal technologies in medicine.
Just as science never stops moving, neither will the funding landscape. As far as Thummel is concerned, “we can learn a lot more by taking advantage of opportunities than we can by resisting change.”

Rutter is used to his ideas being unpopular. Ten years ago, when he started his research lab, few wanted to join, and at times he struggled to cobble enough funding to run it. Rutter had decided to study metabolism, a discipline filled with dizzying mazes of arrows pointing to impossibly long names that many scientists consider to be, well, boring. “At times I had doubts about whether I was doing the right thing,” admits Rutter.
He was convinced, however, that metabolic processes were so fundamental to life they would have to have their fingers in major disease. “I was driven by wanting to be at the forefront, making discoveries that no one else is making,” says Rutter. Years later, he did just that, making discoveries that move us closer to solving a century-old mystery—how cancer cells undergo a metabolic shift that allows them to outpace healthy cell growth. With the help of his now robust research team, Rutter discovered a protein complex critical for converting carbohydrates to cellular energy, and showed it was key to the so-called Warburg effect. They’ve also shown that abnormal tweaks in metabolic pathways contribute to diabetes, among other ailments.
Six major grants, two spin-off companies, and several top-tier publications later, Rutter’s innovative and creative work has become too important to ignore. He is now co-director of the University’s Diabetes and Metabolism Center, co-leader of Huntsman Cancer Institute’s Nuclear Control Program and an HHMI investigator.
Rutter has gone from bucking the trends to setting them, as the once boring metabolism is now red hot. “Now that my field is getting more crowded, I’m starting to think, ‘What’s the next frontier?’” says Rutter. “Maybe, it’s about time to move on and do something different.”

Hearing “quiet” uttered in the same breath as “library” makes Shipman’s hair stand on end. “We’re not a quiet space nor do we want to be,” says the library director. She prefers the excited chatter and hum of groups coming together to share ideas over the pin-drop atmosphere of libraries past. Those bricks-and-mortar libraries once built to be passive repositories of knowledge are no longer needed in today’s dynamic digital information age, says Shipman.
Before Shipman could realize the morphogenesis that had been unfurling in her head she needed to evict its deadweight occupants—books and journals. So starting in January, 2013, the library crew worked at breakneck speed, becoming one of the first academic libraries to replace paper with pixels. Soon their website welcomed 32 million virtual visits to browse more than 36,000 digital journal titles and special collections in a single year.
With the first stage complete, Shipman was free to let her vision take flight. “As library faculty, we are creators of knowledge right along with our student and faculty partners,” says Shipman. She transformed the stack shelving area into a collision space called the Synapse. She invited designers of therapeutic games and health care apps (the GApp Lab) to open shop, and the Center for Medical Innovation to use the liberated space as an incubator for faculty and student start-ups. Together, they’re creating their own ideas and devising new ways to document innovation—an elusive process not captured by traditional journals.
Even as she transforms the space, Shipman’s long-term vision is to have her team fan out across campus, to interact with information in new and exciting ways. “We’ve broken the container of information,” she says. “Now we’re ready to explore everything else that’s out there.”
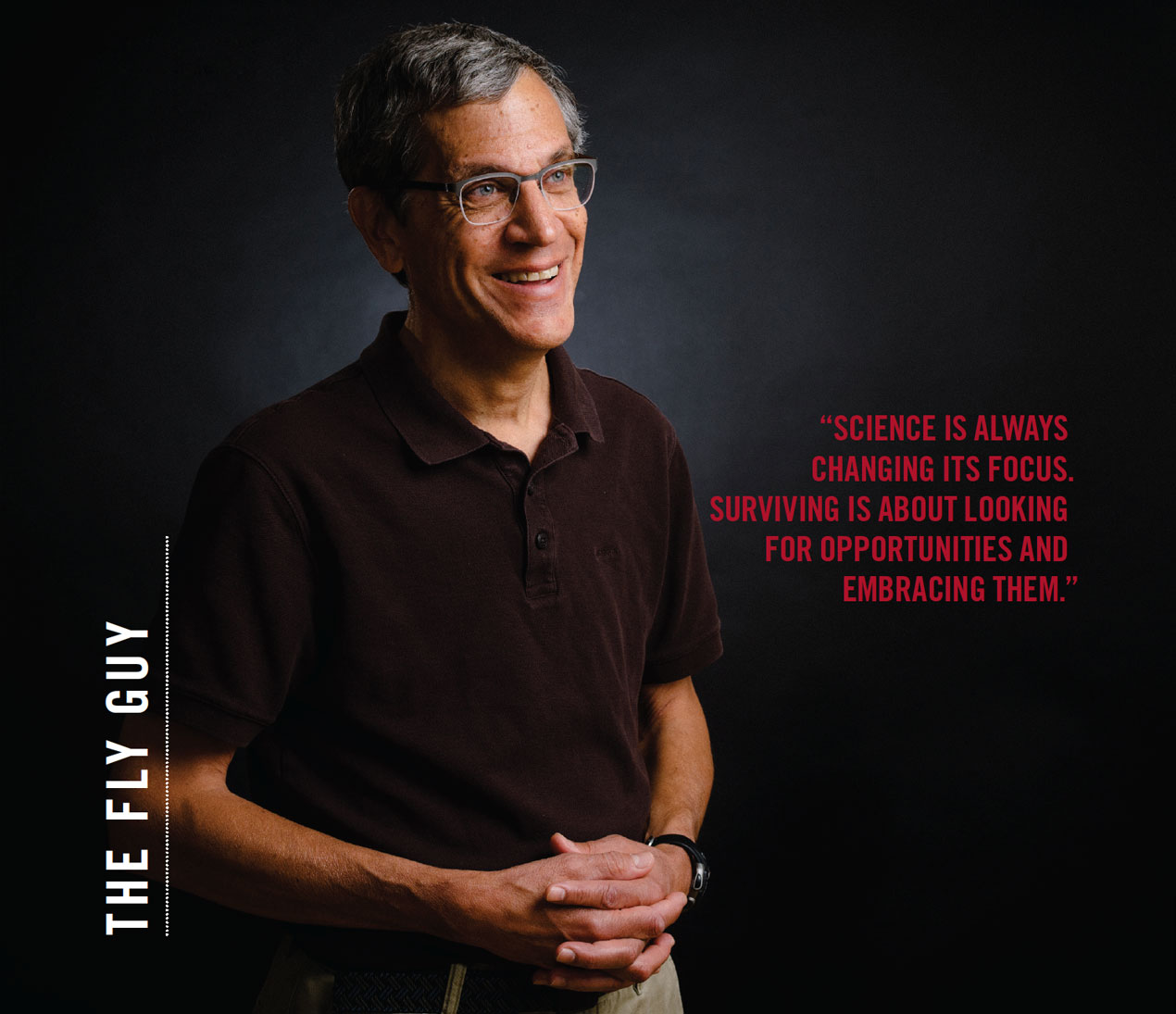
Thummel is well aware that most of his colleagues only think about flies when they have to swat them away. Yet for 100 years, generations of scientists like him have honed Drosophila melanogaster into a data-generating machine. Feed them questions about fundamental biology, and they'll spit out answers with unparalleled speed.
Thummel is used to being the only "fly guy" in the room, but he's not used to being left out of the conversation entirely. That's what happened when his field switched its focus to metabolism. "It's not exactly rocket science to realize that everyone is working on something that I wasn't," says Thummel. The key is not take it personally, he says. "When a field changes you have to change with it. All we had to do was step sideways and do what we already knew but in a different context."
Soon after, one of his experiments turned up flies with the most notorious metabolic disorder-diabetes. "No one expected that something as simple as a fly could have a disease as complicated as diabetes," he recalls. To pursue the research further required that he step sideways once again. He sat down with the chief of endocrinology, metabolism and diabetes and asked: "So what's this insulin thing?" His curiosity sparked an invitation to the division's weekly meetings.
Working with physicians, Thummel has figured out how to diagnose the six-legged animal, even miniaturizing a version of the glucose tolerance test used in clinics. In return, the flies are doing what they do best: revealing previously unknown molecular mechanisms driving the disease. In the wake of these advances, Thummel has become a sought-after expert. "It's been terrifically exciting," he says. "And it's satisfying to know that what we're doing could have a real impact."

It's not every day that a scientist forays into the complicated, time-consuming world of clinical trials. It's much easier to stay in the lab and collaborate with like-minded colleagues.
For Bild, that path was never an option. "Life experiences shape you and help identify what really matters," reflects Bild, who in graduate school helped close family members and friends battle cancer. She knew then that she didn't want her research to live in a journal, she wanted it to help patients fighting for their lives. So when she found evidence that an epilepsy drug, valproic acid, had tumor-fighting capabilities, she assembled the best team-a pharmacologist, medical oncologist and bioinformaticist-to help transform her discovery into a clinical trial.
Bild delved into her teammates' unfamiliar worlds and learned what made them tick. "The advice I have is to learn everyone's perspective and respect what they need," says Bild. Their common goal-to help patients with the greatest possible impact-looked differently to each of them. For the bioinformaticist, it meant making the data and software publicly available. For the oncologist, it meant turning down research ideas that didn't optimize patient care. With that shared understanding, they moved administrative and procedural mountains to make the clinical trial happen.
With the first phase of the Valproic Acid Signature Trial (VAST) complete, data analysis will determine if they're closer to a new treatment for breast cancer patients. "We've been told the way we work together to link the benchwork to the bedside is rare," says Bild. The approach has helped them outcompete some of the nation's top cancer teams for National Cancer Institute support and greased the wheels for further collaboration. "It would be a shame if we didn't do it," says Bild. "We would be missing out on a great scientific opportunity."